Forgive us, for this is a long one, though we think it is well worth it. It’s a little rough at the end. We will apologize next month.
A few weeks ago, DS started advertising with Google.
Our phone calls and emails have increased dramatically. Most of the calls are from elderly people who need help. More specifically, FREE help from the Ontario Government. “You know”, they would say, ”like before”. “Yes”, I say, “I remember it well”.
One call last week was from an elderly woman, let’s call her Georgia, who was sent home from her local emergency department. She had fallen and hit her head. Once they tended to her cuts, they sent her home telling her to “call for help.” Not a lot of detail there but she found our number and wanted her “free” help.
She indicated that she was looking for 10 hours of daytime help. We directed her to call the main number for HCC (“Home and Community Care Support” formerly the LHIN, Local Health Integrated Network. No one knows why they keep changing the acronym, but every change reduces resources.) By the way the main number is 310-2222 no area code needed. We gently tempered her expectations for receiving the level of care she felt she needed. She called HCC, was given an appointment for an assessment in the middle of the following week and was told that she could get help for a weekly shower starting the next day. She said that she needed help now. They indicated that she could always for pay for private care. She called me back. I advised her that 10 hours a day at an average of $32.00 an hour would cost her $2240.00 per week.
She was gobsmacked. I asked if she had any children, she said no. I asked if she had any friends or other family members she could ask for help. I could hear her roll her eyes…what is there to do? There are not a lot of people available to provide free care to elderly people in need.
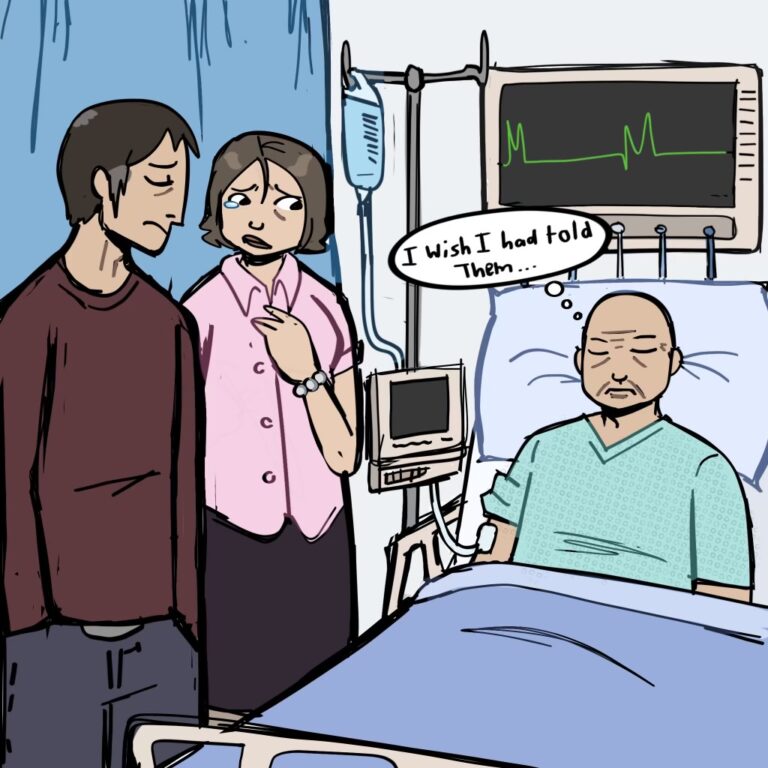
In all honesty, this problem is not going to go away for her, is it? It is just going to get worse – not only for her but for tens of thousands if not hundreds of thousands of people.
That is, until she gets to a point in her life when her death is more or less imminent, and then sadly there is help available. (More on that in a later blog.)
But what about that in-between part? What is going to happen to Georgia and all the others? Every day, there are stories about how our health care system is on the brink of collapse. And in Ontario, there doesn’t appear to be an answer – in fact recent government ads encourage people to talk to their health care providers more, this while millions have no GP to call.
The truth is we need to re-define health care HONESTLY and address the issues HONESTLY. Unfortunately, the whole thing comes down more older people, less money for the healthcare services that are needed.
Let’s take a look at the numbers.
We’re living longer
In 1947 when Tommy Douglas introduced the first provincial hospital insurance program in Saskatchewan, the average life span was roughly 64 years old. To put that in perspective, people were not eligible for OAS (Old Age Security) until they were 70 (unless they were blind then they could get OAS at 40). No other physical or mental challenge – just blindness. (Strangely specific.)
Of course, things like infant mortality and other deadly childhood diseases like measles and polio brought the life expectancy average down but still, people got sick (cancer, heart disease, lung disease) and died. They rarely lingered for decades and if they did there was a woman at home ready to provide the needed care.
Today we have largely eradicated childhood diseases (in spite of the anti-vaxxer efforts to make death by childhood diseases great again) and as adults we can survive and continue living with diseases that were once a death sentence. But while we continue to extend life, it is important to know that the quality of that extended life can sometimes be questionable. Additionally, there is no way the system can continue to provide the chronic self or personal care that people have come to expect.
Stats Can places life expectancy in Canada now at 81.7 (we took a bit of a hit with COVID) it was closer to 84 for men and 86 for women. And if you have lived to age 70, the odds are very high that you will live to the age of 86 (at least), and the higher your income and education levels are, the more likely you are going to reach 100 (statistically).
Now, that does not mean that you will be running marathons at 100, but you will still be breathing, you could be on oxygen but you will still be here.
Why the shortfall in services?
For decades, our provincial governments have avoided telling us that healthcare will be unaffordable for most. Why is that? We think it’s because this issue primarily affects older people, and the majority of older people vote, and no one wants to offend them.
Instead of levelling with us they throw numbers at us. The Federal Government will be investing $198.6 billion dollars over the next ten years, and they have increased that an additional $46.2 billion in new support, and because those numbers sound huge, we assume it is enough. It is not. Yes, you read that correctly. Demand will exceed supply by 2028. Let’s look at some statistics.
According to the Financial Accountability Office (“FAO”) of Ontario’s March 8th, 2023, summary of planned health expenditures: “the Province has committed to make significant investments to expand capacity in hospitals, home care and long-term care. However, these increases in capacity will be more than offset by increases in demand for these services from Ontario’s growing and aging population. Relative to projected growth in demand, by 2027-28, Ontario will have less hospital capacity, similar home-care capacity and less long-term care capacity compared to what it had in 2019-20.”
Furthermore, the FAO predicts the current shortage of nurses and PSWs will continue, with a shortfall of 33,000 nurses and PSWs by 2028. This shortage will undermine Ontario’s ability to sustain programs, let alone fulfill expanded commitments to new programs. This means that the oft-promoted “age at home” idea will have to be done with virtually no publicly funded assistance (ie/ no free personal support workers.)
On top of all that, the province is underfunding its commitments to health sector programs and its commitments to hospitals, home care and long-term care by $21.3 billion, according to the FAO. This sadly will result in more program cuts and less resources, despite the additional federal funding.
The Last Word
Currently there is a shortfall in what is provided versus what is needed and going forward the Ontario Government’s plan for healthcare is not going to work. We’ll need more funded services, nurses and PSWs, not less.