Today’s blog will be the first of a series describing the journey through the healthcare system as an aging Canadian. For the purposes of privacy, names and circumstances have been altered slightly. Through sharing this experience, we hope to help you better navigate your own journey when the time comes, so you can be less fearful and better equipped to handle whatever comes your way.
Frank is in his 80’s and suffering from two late stage cancers. While initial diagnosis was grim, a few months at most, Frank underwent cutting edge cancer treatment through St. Margaret’s Hospital and was gifted a decade more time to spend with family and friends. Frank was lucky to live with family next door who were able to accommodate his doctor’s appointments, some taking several hours at a time. As his health began to decline, he was advised to discontinue his cancer treatment as it was too invasive and the risk benefit ratio was considered poor. A series of mini strokes followed. Initially his family thought they were fainting episodes and a number of tests were inconclusive. Each episode meant he was admitted to hospital by ambulance to the ER, and each time he was discharged home after his vitals were settled. The ER is no place for an elderly man with chronic healthcare problems. The family experienced a revolving door between home and the ER.
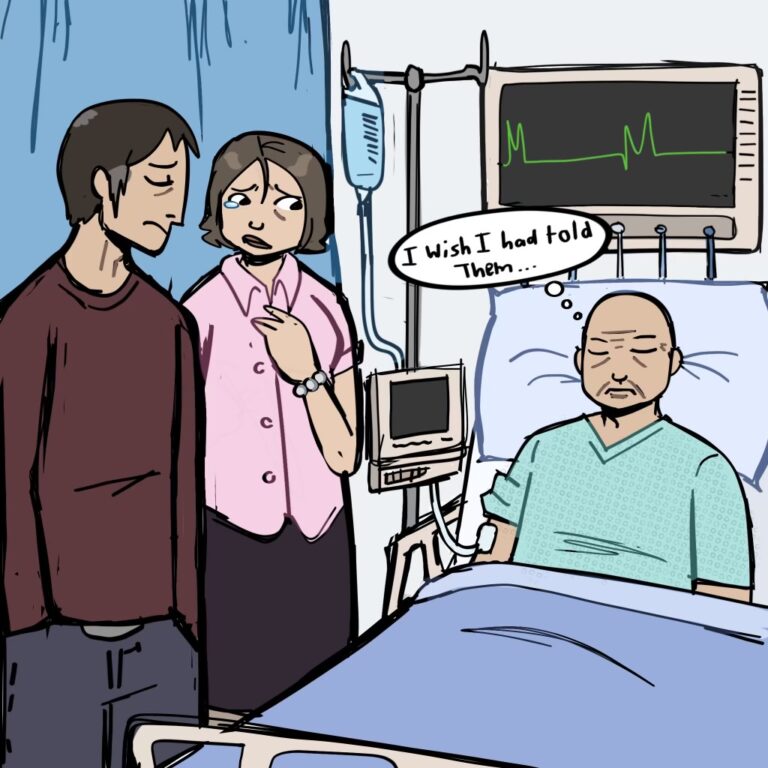
You’ll notice that no comprehensive plan was drawn up between healthcare practitioners and the family. Not because staff and family didn’t care, more because of the lack of clear communication between all the moving parts of complex eldercare. Plus, emergency rooms are overflowing with non-emergency cases, meaning there was very little time to balance his needs. Compounding this is the the fact that Frank’s GP had retired (1.8 million Canadians are without a GP according to the Ontario College of Family Physicians). Perhaps if he had a GP a more comprehensive plan could have been drawn up and communicated which may have resulted in a better experience for all. Frank’s health continued to decline slowly. Initially he was assessed by a social worker and put on a Long-Term Care home waiting list. Sadly, no one from Home and Community Care Support Services (the government agency responsible for access to Long-Term Care homes) followed up to continue to monitor his progress. Any further care was provided by his family who tried to patchwork where OHIP leaves off, using personal funds for a night nurse.
When he could no longer remain at home due to being bed-bound and needing help with toileting, but not having access to a Long-Term Care home, Frank was then in a veritable no man’s land. It’s at this point that care becomes difficult to find. Frank’s family scrambled between rehab centres and the ER several times. Distraught over the shambolic care of Frank, the family continued to advocate on his behalf, constantly updating new nurses and doctors of his previous care issues. No wonder Frank fell through the cracks, along with his family and the medical staff.
We can and need to do better. Frank’s story is not unique and we know all of you reading this will see your own stories reflected. The question is: what do we DO about it?
Over the next few months we will help you understand the limitations of our healthcare system and we will outline where the system pauses care, where individual responsibility lies, and when the system steps in again. We will describe opportunities to lessen anxiety and describe steps that can be taken to support our loved ones.
Healthcare is more than the absence of disease, it is also the presence of peace of mind that Discerning Seniors can help provide your family. We will address each of the missed opportunities to improve Frank’s experience in our next newsletter/blog.